What is a fungal nail and what causes it?
Onychomycosis, or fungal nail infection as it’s more commonly called, is a common nail condition. It occurs as a result of a dermatophyte fungal infection affecting the nail plate. While fungal nail infections are mostly considered an aesthetic issue, they can lead to ulcers in the diabetic population, and cellulitis in older adults (Westerberg & Voyak 2013). Further, they can have a significant impact on activities of daily living in the general population.
Who do fungal nails affect?
Fungal nails affect people of all ages, however it is the elderly population that is most affected. The prevalence of fungal nail infections increase with age, occuring in 10% of the general population, 20% of the population aged older than 60 years, and 50% of those aged over 70 years (Thomas et al. 2010). This increased prevalence in older populations is primarily linked to the higher incidence of diabetes mellitus, immune disorders, and peripheral vascular disease (Westerberg & Voyak 2013).
Although it is primarily those aged above 70 years who are at most risk, those with diabetes are up to 2.8 times more likely to develop a fungal nail infection (Mayseret al. 2009). Smokers, people who use occlusive footwear, and those who use shared shower facilities are also at increased risk of developing fungal nail infections (Westerberg & Voyak 2013).
What are the symptoms of a fungal nail infection?
Depending on the type and severity of the fungal infection the associated symptoms and clinical presentation may differ.
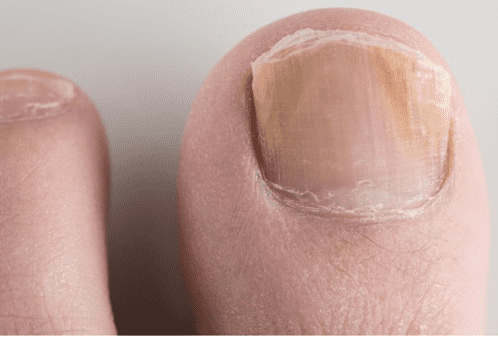
A superficial infection only affects the outermost layers of the nail plate. This type of infection will typically present as opaque white patches distributed across the top layers of the nail. Typically these white patches will increase in size and spread as the infection progresses (Elewski 1998).
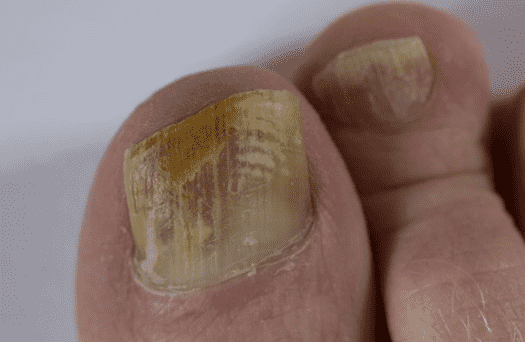
In more severe cases, the fungal infection will commonly cause the nail to become thickened and detached from the nail bed. Once detached, fungi is able to enter under the nail plate causing a yellowish brown discolouration to the nail (Thomas et al. 2010).

How do we treat fungal nails?
Fungal nail infections are often difficult to treat as toenails typically grow very slowly and receive little blood supply. However, there are still treatment option available which vary in efficacy depending on the severity of infection. The three most common treatment options include, topical treatment, oral systemic treatment, and laser therapy.
Topical treatments are most suitable for minor and superficial fungal nail infections. They are the least effective form of treatment and are limited by their inability to penetrate into the the deeper infected layers of the nail plate. As a result topical treatments are best suited for very superficial infections, or as an adjunct therapy in more severe cases (Bala & Taher 2013).
In the case of more severe fungal nail infections, oral medications are often a more appropriate treatment method, especially when compared to topical options. Oral medications are able to move systemically through the body in order to penetrate the nail plate, resulting in higher cure rates. However, oral antifungal medications are not suitable for all patients. While there may be few contraindications between other medications, they are not recommended in patients with liver disease, or heart failure. These medications also somewhat inconvenient as they are taken over a three month period, and require blood tests to assess liver function along the way (Bala & Taher 2013).
In recent years laser therapy has become the most recommended course of treatment for fungal nail infections. During laser therapy a laser beam penetrates the entire nail plate and disrupts the fungal spores, resulting in their death (Bala & Taher 2013). Laser therapy is an effective and convenient method of treatment for all forms of fungal nail infections.
References
Bala, AD & Taher, A 2013, Onychomycosis and Its Treatment, International Journal of Advances in Pharmacy, Biology, and Chemistry, vol. 2, no. 1, pp. 123-129.
Elewski, BE 1998, Onychomycosis: Pathogenesis, Diagnosis, and Management, Clinical Microbiology Reviews, vol. 11, no. 3, pp. 415-429.
Mayser, P, Freund, V & Budihardja, D 2009, Toenail onychomycosis in diabetic patients: issues and management, American Journal of CLinical Dermatology, vol. 10, no. 4, pp. 211-220.
Thomas, J, Jacobson, GA, Narkowicz, CK, Peterson, GM, Burnet, H & Sharpe, C 2010, Toenail onychomycosis: an important global disease burden, Journal of Clinical Pharmacy and Therapeutics, vol. 35, no. 5, pp. 497-519.
Westerberg, D & Voyak, MJ 2013, Onychomycosis: Current Trends in Diagnosis and Treatment, American Family Physician. Vol. 88, no. 11, pp. 762-770.
