Several common causes of shoulder pain can be successfully treated and managed with physiotherapy. Our top 5 common presentations for shoulder pain to the clinic are listed below; some other causes were close but didn’t quite make this list! So, you must consult with your physiotherapist or medical professional if you suffer from shoulder pain.
Shoulder Impingement
What is Shoulder Impingement?
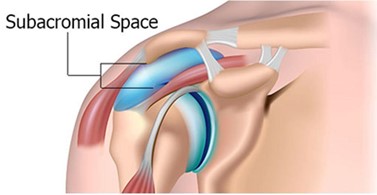
Shoulder impingement is perhaps the most common shoulder condition seen in clinics. As pictured, the subacromial space is formed between the acromion and the head of the humerus; some critical structures lie in this small space. The rotator cuff tendons pass through this space, compressing the humerus to keep the shoulder joint stable. The sub-acromial bursa is a fluid-filled sac that reduces friction between muscles and tendons moving against the bones. During shoulder elevation, either one or both structures can be compressed between the humerus and the Acromion, referred to as shoulder impingement.
Who Suffers From Shoulder Impingement?
Those who perform repeated overhead movements are more likely to develop shoulder impingement. This may be exhibited in throwing athletes, swimmers, weightlifters, tennis players, or golfers in the younger population. Older people may see it as manual labour workers, painters, and carpenters, but it is not limited to this population.
What Causes Shoulder Impingement?
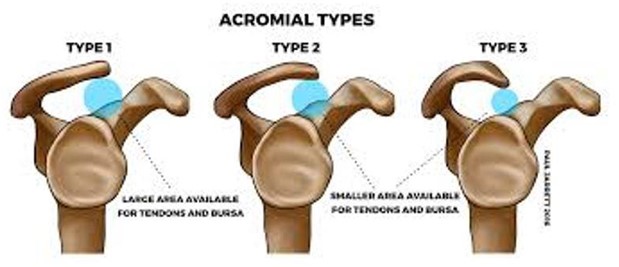
Many factors can contribute to the development of shoulder impingement. The research has classified these factors as primary or secondary causes of shoulder impingement. Direct impingement refers to the structure of one’s shoulder anatomy. Some people are born with a hooked acromion, as pictured below; this reduces the sub-acromial space and may increase the likelihood of developing impingement. Degenerative conditions such as osteoarthritis may lead to the development of bony spurs, which also narrow the sub-acromion span and contribute to shoulder impingement.
Secondary impingement addresses biomechanical factors that contribute to the development of shoulder impingement. These are the factors your physiotherapist is trained to assess and treat. These may include a lack of rotator cuff strength or rotator cuff tendon pathology, poor scapular stability or motor control, shoulder instability, biceps tendon pathology, or a lack of shoulder and thoracic mobility.
What is the Treatment for Shoulder Impingement?
Physiotherapy is highly indicated for diagnosing and treating shoulder bursitis. The early stages of physiotherapy therapy treatment will aim to alleviate the irritability and severity of symptoms. This may involve your physiotherapist suggesting or implementing a combination of the following:
- Rest
- Ice
- Anti-inflammatories
- Activity modification
- Taping
- Soft tissue massage
- Dry needling
Your physiotherapist will also assess the biomechanics contributing to your shoulder impingement. Given the numerous factors leading to shoulder impingement, treatment may vary considerably between cases. Therefore, understanding the biomechanics related to your impingement is vital. Once the initial irritability has settled, your physiotherapist will provide a personalised treatment plan that may address a combination of the following:
- Rotator cuff strengthening
- Scapulothoracic musculature strengthening
- Dynamic scapular control
- Shoulder/thoracic mobility
- Posture correction
Shoulder Bursitis
What is Shoulder Bursitis?
Shoulder bursitis is a painful condition resulting from inflammation of the bursae of the shoulder. Bursae are fluid-filled sacs that can be found surrounding joints and bony prominences all over our body. They facilitate movement by acting as a cushion to reduce the friction between tendons, ligaments, and bones. The main shoulder bursae are:
- Subacromial Bursa
- Subdeltoid Bursa
- Subscapular Bursa
- Subcoracoid Bursa
The sub-acromial bursa is the most affected bursa of the shoulder. In shoulder bursitis, the bursa is compressed during shoulder elevation between the acromion process and either the rotator cuff tendons, humeral head, or coracoacromial ligaments.

Cause of Bursitis
Shoulder bursitis is closely related to shoulder impingement, as any impingement in the shoulder will likely result in compression of the bursa.
Most cases of shoulder impingement present as chronic, overuse-type injuries. Bursitis is common in those who perform repeated overhead, such as painters, tennis players, or basketballers. Certain biomechanical factors may predispose individuals to developing bursitis, and wsothe pain disappears. These factors may include:
- lack of rotator cuff strength or rotator cuff tendon pathology
- poor scapular stability and motor control
- shoulder instability
- biceps tendon pathology
- lack of shoulder and thoracic mobility
Less commonly, bursitis can present as an acute injury. This may result from a fall or direct trauma to the shoulder. This could be seen in the elderly population after a fall, in racquet athletes, or contact sports. It is essential in these cases that fractures, rotator cuff tears, and dislocations are first excluded before proceeding with treatment.
What is The Clinical Presentation of Shoulder Bursitis?
People complain of pain in the front or outside of the shoulder, which may extend as low as the elbow.
As many cases are partly due to overuse, shoulder pain may begin as a dull ache when lifting the arm. Gradually, this pain may worsen over the coming weeks or months, becoming more consistent and possibly associated with a loss of strength or range of motion.
Activities involving raising the arm, such as combing your hair, hanging out, washing, or reaching the top cupboard, aggravate symptoms. Laying on the affected component may also exacerbate the symptoms.
The painful arc, as pictured below, is a crucial sign of shoulder bursitis. This is where pain is at its worst, approximately between 60 and 120 degrees of shoulder elevation, and above this range, pain is alleviated. This is due to the pressure placed on the bursa through this range; pain subsides as the arm is raised further and pressure is lessened.

Shoulder Bursitis Treatment
Physiotherapy Adelaide is highly indicated for diagnosing and treating shoulder bursitis. The early stages of physiotherapy therapy treatment will aim to alleviate the irritability and severity of symptoms. This may involve your physiotherapist suggesting or implementing a combination of the following:
- Rest
- Ice
- Anti-inflammatories
- Activity modification
- Taping
- Soft tissue massage
- Dry needling
- Shoulder and scapular strengthening programming
In the long term, a graded exercise program is highly effective in alleviating symptoms and reducing the recurrence of shoulder bursitis by addressing the underlying biomechanical factors previously discussed. A biomechanical assessment is necessary to develop an appropriate exercise plan to understand the factors contributing to your bursitis.
Cortisone injections are a valuable tool to reduce pain caused by bursitis quickly. However, they are often a short- to medium-term ‘ solution’ as the underlying cause of the impingement has not been addressed. In almost all cases where cortisone is indicated, the optimal treatment would be to follow up with a course of Physiotherapy and exercise program.
Rotator Cuff Tears
What is a Rotator Cuff Tear?
A rotator cuff tear is a tear in the muscles of the shoulder blade. Most commonly, the supraspinatus muscle or tendon is not limited to that. We see rotator cuff tears in approximately 50% of all significant shoulder injuries, but they are not always the cause of the person’s symptoms. The muscles work together in a group as they form a cuff around the head of the humerus (upper arm bone), and when working in sync, they allow you to lift and rotate your arm; they also have a critical role in ensuring the arm bone does not clash with the bone that overhangs it, called the Acromion. When dysfunction in muscle patterning occurs, you develop impingement in the shoulder and, over time, with repetitive stress and trauma, other issues such as bursitis and rotator cuff tears.
What Causes Rotator Cuff Tears?
Rotator cuff Tears can be caused by trauma and non-trauma events. A significant fall can cause a tear, or a shoulder dislocation or subluxation can do this and result in an acute traumatic tear. However, we also see these types of tears progressing quietly and subtly over time in people; most people will never experience symptoms from them; however, a percentage of the population will.

A study published in the Journal of Shoulder and Elbow Surgery found that in their population sample across the lifespan, 23% of patients had evidence of rotator cuff tears on imaging studies.
In group 1 (aged 50 to 59 years), 13% (22 of 167) of the patients had tears.
In group 2 (aged 60 to 69 years), 20% (22 of 108) of the patients had tears.
In group 3 (aged 70 to 79 years), 31% (27 of 87) of the patients had tears.
In group 4 (age >80 years), 51% (25 of 49) of the patients had tears.
Aspects that may increase your chance of developing a rotator cuff tear are:
- Bone spurs under the Acromion
- Reduced Blood Supply to the area (smokers, particularly)
- Repetitive loading or stress to the site over time
This shows that the prevalence of rotator cuff tears increases as we age and can be deemed a regular part of aging. Rotator cuff tears can also be of different degrees, ranging from minor partial-thickness tears to major total-thickness tears.
What is The Treatment For Rotator Cuff Tears?
Your physiotherapist can work with you on the best way to treat and manage your rotator cuff tears. Most tears can be treated with conservative management (physiotherapy); however, surgical repair can be indicated if the injury does not respond to conservative management very well.
- Rest
- Ice
- Anti-inflammatory medications
- Activity modification
- Taping
- Soft tissue massage
- Dry needling
- Shoulder and scapular strengthening programming
- Surgical repair, where indicated
Similarly to impingement and bursitis, a graded exercise programme is highly effective in alleviating symptoms and reducing the recurrence of rotator cuff injuries in the long term. A biomechanical assessment is necessary to develop an appropriate exercise plan to understand the factors contributing to your rotator cuff tear. A cortisone injection can be helpful in this type of injury to reduce very acute pain and inflammation if more conservative management and measures fail. However, recurrent long-term cortisone injections are not supported and should be avoided to minimise more long-term pain disability and potential ongoing degradation of the tendon tissue.
Rotator Cuff Strain or Rotator Cuff Tendonitis Rotator Cuff Tendinopathy)
Rotator cuffs do not always tear! They can become strained or inflamed and are usually more difficult to treat conservatively. These strains or inflammation of the tendon are often referred to as rotator cuff tendonitis or rotator cuff tendinopathy, which physiotherapy treatment is highly effective in addressing.
Shoulder Arthritis
Regarding shoulder arthritis, we see a couple of standard forms affect the shoulder the most. At its core, arthritis is the inflammation of a joint. However, the two forms of arthritis that affect the shoulder the most are osteoarthritis and rheumatoid arthritis.
OSTEOARTHRITIS (OA)
This form of arthritis affects the smooth cartilage (hyaline cartilage) on the ends of bones, where they become joints and interact with another joint surface. This form of arthritis, when present, reduces the smoothness of the bony surfaces and exposes the skinny layer underneath. Over time and with ongoing movement, this degradation slowly continues and progresses. Worsening osteoarthritis in the joint usually leads to increased inflammation and, sometimes, pain from just resting the shoulder. Morning stiffness and a loss of overall shoulder range of motion are usually signs of this as well. It can sometimes affect sleep by making you unable to lie on the shoulder.
RHEUMATOID ARTHRITIS (RA)
Rheumatoid arthritis is an inflammatory form of arthritis that is systemic and is caused by an autoimmune response in the body. The autoimmune reaction is when the body attacks itself. In the case of the shoulder, it attaches to the synovium, or joint lining. The synovium is a structure found in the lining of joints responsible for producing synovial fluid, which lubricates the joints. Rheumatoid arthritis often affects multiple joints, often on both sides. It is most commonly seen in the hands and will most often affect both sides of the shoulders.
Frozen Shoulder Or Adhesive Capsulitis
What is frozen shoulder or adhesive capsulitis?
People with frozen shoulder or adhesive capsulitis often have stiffness and inflammation around the surrounding shoulder capsule. These are the ligaments that allow the shoulder to move freely. When they become thickened and tight, they restrict this movement and function quite heavily.
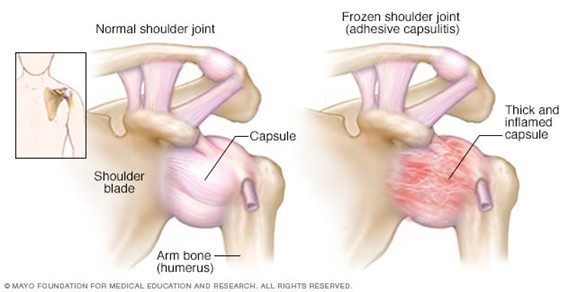
There are often three stages of a frozen shoulder, and treatment varies at each location.
Stage 1: Freezing (0–6 months)
The freezing component of the frozen shoulder can last for approximately six months and is usually quite a painful part of the injury. Interventions that can be utilised at this stage of the disease are anti-inflammatory medication and pain medication. There is also an indication for the use of cortisone injections and potentially hydro dilatation injections, which can be quite helpful in preventing or halting the disease progression. Physiotherapy combined with these can help maintain the shoulder’s range of motion and assist in pain management.
Stage 2: Frozen (6–12 months)
During this phase of the frozen shoulder, pain is often minimal, and loss of range of motion is at its maximum. Usually, you are left with a shoulder that feels like you cannot move past specific fields.
Physiotherapy treatment in this phase is essential to maintain the strength of the shoulder and the muscles around it. It is also necessary to allow for gradual regaining of the range of motion over time. It can also help with general muscular stiffness of the upper back, arm, and neck that might be encountered from a lack of overall movement.
Stage 3: Thawing (12–18 months)
This is the disease’s final phase and is usually associated with a progressive increase in range of motion and regaining of strength.
It is important to note that this condition can affect almost anyone. However, it is most commonly seen in females aged in their 40s and those who may have some form of systemic disease such as diabetes or prediabetes. It can also occur in some people as a post-operative complication, especially after immobility.




